ARTICULO ORIGINAL
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2021 - Universidad Ricardo Palma10.25176/RFMH.v22i1.4383
SCHEME OF INTERMITTENT FASTING AND REDUCTION OF ANTHROPOMETRIC MEASURES, LIPID PROFILE, BLOOD PRESSURE AND CARDIOVASCULAR RISK
ESQUEMA DE AYUNO INTERMITENTE Y REDUCCIÓN DE MEDIDAS ANTROPOMÉTRICAS, PERFIL LIPÍDICO, PRESIÓN ARTERIAL Y RIESGO CARDIOVASCULAR
J. Javier Wong-Gonzales 1 , José Antonio Quispe-Palacios 1
1 Faculty of Human Medicine, Universidad Ricardo Palma. Lima Peru
ABSTRACT
Introduction: Lifestyle is a fundamental role in the risk of cardiovascular diseases and chronic diseases. Objective: To evaluate the effect of the 16/8 intermittent fasting scheme against anthropometric measurements, lipid profile values, blood pressure and cardiovascular risk. Method: Longitudinal analytical study with intervention. Fifteen patients treated in the nutrition area in a private center between January and October 2020 submitted to the 16/8 intermittent fasting scheme for four months, seeking to reduce anthropometric measurements, lipid profile, blood pressure and / or cardiovascular risk. Variables: body weight, body mass index (BMI), waist-hip index (WHI), abdominal circumference, lipid profile, cardiovascular risk according to Framingham (Framingham AMR B table), total cholesterol / HDL and LDL / HDL indices. Results: The average age was 47.1 years, the average height was 1.66 m., The average body weight was 84.3 Kg., The average of the BMI was 30.46, the average of the WHI was 0.94, the average of the abdominal circumference was 99.87, the mean total cholesterol, HDL and LDL were 240.06, 43.73 and 153.2 respectively, the mean cardiovascular risk according to Framingham was 0.11% and the mean total cholesterol / HDL and LDL / HDL indices were 5.88 and 3.69. The evaluation of averages before and after found significant differences (p < 0.05) at 3 and 4 months of evaluation. Conclusions: The intermittent fasting scheme showed a significant reduction in anthropometric measurements, lipid profile and cardiovascular risk. Additionally, an increase in HDL was observed.
Keywords: Intermittent fasting, body weight, body mass index, blood pressure, lipid profile. (Source : MeSH - NLM).
RESUMEN
Introducción: El estilo de vida juega un rol fundamental en el riesgo de enfermedades cardiovasculares y enfermedades crónicas. Objetivo: Evaluar el efecto del esquema de ayuno intermitente 16/8 frente a las medidas antropométricas, valores de perfil lipídico, presión arterial y riesgo cardiovascular. Método: Estudio analítico longitudinal con intervención. Quince pacientes tratados en el área de nutrición en un centro privado entre enero y octubre del 2020 sometidos al esquema de ayuno intermitente 16/8 por cuatro meses, buscando la reducción de medidas antropométricas, perfil lipídico, presión arterial y/o riesgo cardiovascular. Variables: peso corporal, índice de masa corporal (IMC), índice cintura – cadera (ICC), circunferencia abdominal, perfil lipídico, riesgo cardiovascular según Framingham (tabla de Framingham AMR B), índices colesterol total/HDL y LDL/HDL. Resultados: La edad promedio fue 47.1 años, la talla promedio fue 1.66 m., el peso corporal promedio fue 84.3 Kg., el promedio del IMC fue 30.46, el promedio del ICC fue 0.94, el promedio de la circunferencia abdominal fue 99.87, el promedio del colesterol total, HDL y LDL fue 240.06, 43.73 y 153.2 respectivamente, el promedio del riesgo cardiovascular según Framingham fue 0.11% y el promedio de los índices colesterol total/HDL y LDL/HDL fue 5.88 y 3.69. La evaluación de promedios antes y después encontró diferencias significativas (p < 0.05) a los 3 y 4 meses de evaluación. Conclusiones: El esquema de ayuno intermitente mostró reducción significativa de las medidas antropométricas, perfil lipídico y riesgo cardiovascular. Adicionalmente se observó aumento del HDL.
Palabras Clave: Ayuno intermitente, peso corporal, índice de masa corporal, presión arterial, perfil lipídico. (Fuente: DeCS BIREME).
INTRODUCTION
Intermittent fasting or intermittent food restriction (RAI), as it is also known, is a lifestyle
approach applied to individuals whose objective is mainly the regulation of body weight(1). The evidence shows that the practice of RAI has favorable repercussions on
health; not only because of the progressive weight loss, but also because of the consequence it has on
the muscular system(2). That is to say, it implies a benefit on the
metabolism. Some authors affirm that this practice also has a positive effect on other health
conditions, including the value of blood pressure, lipid profile and muscle mass index (BMI).
Harmful habits, unhealthy eating, sedentary lifestyle, insufficient sleep, among others, will
lead to obesity, high blood pressure, dyslipidemia; all of them will lead to an increase in
cardiovascular risk and, therefore, the propensity to suffer a cardiovascular event(3,4).
According to the WHO, in 2011, there were around 17 million individuals who died from some
cardiovascular disease (29.82%) and it was estimated that for the present (2020) this number would
increase by 15 to 20%. Also, it was predicted that by 2030 around 23.6 million individuals will die;
this being the main cause of death worldwide(5).
In Peru, after a study conducted in which cardiovascular risks versus risk factors were
addressed in a hospital in Lima, it was found that a large percentage of the individuals evaluated
suffered from obesity and / or diabetes mellitus; both are metabolic disorders that lead to increased
cardiovascular risk(6)
Due to the aforementioned, the objective of this study is to evaluate the effect of the 16/8
intermittent fasting scheme against anthropometric measurements, lipid profile values and cardiovascular
risk.
METHODOLOGY
Design and study area
An analytical, longitudinal study with intervention was used in patients attending the nutrition area of a private health center in metropolitan Lima, Peru.
Population and sample
After a previous explanation of the intervention, patients treated in a nutrition area clinic in a private health center, who had not obtained adequate results with traditional nutrition methods prior to the tests, were invited to perform the 16/8 intermittent fasting scheme after prior explanation of the intervention. months of January and October 2020, of which fifteen patients agreed to participate for 4 months. The recommendation was given by a qualified nutritionist, who, in turn, prescribed a dietary structure for each of the patients according to his requirements; that is, whether the patient was seeking weight reduction, lipid profile reduction, blood pressure reduction or increase in muscle mass. Those patients younger than 20 years and older than 70 or patients with chronic renal failure (CRF) were excluded; as well as those who decided not to participate in the scheme.
Variables and instruments
The variables considered in the study are smoking, weight, body mass index, waist-hip index (ICC), abdominal circumference, lipid profile, in which the values of HDL, LDL and total cholesterol, systolic blood pressure (SBP) and diastolic blood pressure (DBP), cardiovascular risk obtained as a percentage from the Framingham AMR B risk table, which is a variant of the Framingham table that is applied in the Latino population. The risk index for coronary heart disease (I.R.E.C) was also used, which includes I.R.E.C * (total cholesterol / HDL cholesterol index) and I.R.E.C ** (LDL cholesterol / HDL cholesterol index).
Criteria evaluated in the Framingham AMR B table
Age
Diabetes
Smoking habit
Total cholesterol
HDL cholesterol
Systolic blood pressure (SBP) by sex
Diastolic blood pressure (DBP) by sex
All participants had an exhaustive evaluation of anthropometric measurements using a calibrated
mechanical scale from the nutrition office to obtain the patient's weight. There was also a height rod
incorporated into the scale to obtain the patient's height. With the two previous values, the BMI was
obtained. The waist-hip index was found after obtaining the perimeter of the waist using a tape measure;
as well as the size of the hip circumference. The abdominal circumference was also obtained by using a
tape measure according to the WHO recommendations. The lipid profile, where the values of HDL, LDL and
total cholesterol were obtained, was measured through a biochemical examination with enzymatic and
colorimetric techniques within the facilities of the private center. The blood pressure of each of the
patients was measured through the repeated use of an analog sphygmomanometer and stethoscope.
Procedures and intervention
The fifteen patients underwent the 16/8 intermittent fasting scheme for four months. The
measurement of the previously mentioned variables was carried out once the study period had ended. The
follow-up of each of the patients was monthly or bimonthly according to the request of the nutritionist.
Due to the state of emergency, part of the follow-up was carried out through teleconferences in which
the patient had to report her weight at that time; as well as, the waist, hip and abdominal
circumference.
Additionally, it was considered if the participant used tobacco at the beginning of the scheme,
if he suffered from any comorbidity or if he was medicated with some type of drug.
Carrying out this particular intermittent fasting scheme consists of 16 hours of uninterrupted
fasting and 8 hours where the participant is allowed to eat food according to the type of diet that the
nutritionist has determined; the latter could be hypocaloric, normocaloric or hyperproteic.
Statistical analysis
The effect of the 16/8 scheme of intermittent fasting on the previously mentioned variables was evaluated using the finding of the arithmetic mean or sample mean in each of the variables considered. Likewise, the absolute value was found; as well as, the proportion of variation between the initial data and final data. Additionally, the p value of each variable was found by means of the Student's t statistical test for means of paired samples provided by the Excel program; as well as the Chi square statistical test to compare prevalences of the different parameters evaluated before and after the program.
Ethical issues
Both the author and co-authors state that they have no conflicts of interest after conducting this study. The study respects the privacy and confidentiality of the personal data of each of the participants. The Declaration of Helsinki guidelines for research in humans were met.
RESULTS
Prior to performing the 16/8 intermittent fasting scheme, the mean and standard deviation obtained from the fifteen participants were: for age it was 47.1 years ± 11.4; for height it was 1.66 meters ± 0.10; for initial body weight it was 84.3 ± 17.6 Kg; for BMI it was 30.4 ± 5.14 Kg / m2; ICC was 0.9 ± 0.05; for abdominal circumference it was 99.8 ± 10.6; for total cholesterol, HDL and LDL were 240.0 ± 42.8, 43.7 ± 10.6 and 153.2 ± 43.8 respectively. For cardiovascular risk according to Framingham it was 12.0% ± 0.09 and total cholesterol / HDL and LDL / HDL indices of 5.88 ± 2.16 and 3.6 ± 1.3 respectively. In addition, it was established whether or not the participant was a smoker; the type of diet recommended; as well as whether or not they had diabetes mellitus Table 1.
Table 1. General characteristics of the patients.
| Frequency | Percentage | |
|---|---|---|
| Sex | ||
| Male | 8 | 53.3 |
| Feminine | 7 | 46.7 |
| Age* | 47.1 | ± 11.4 |
| Smoker | ||
| Yes | 2 | 13.3 |
| No | 13 | 86.7 |
| Size | 1.66 | ± 0.10 |
| Diabetes mellitus 2 | ||
| Yes | 2 | 13.3 |
| No | 13 | 86.7 |
| Type of diet ** | ||
| Normocaloric | 2 | 12.5 |
| Hypocaloric | 10 | 62.5 |
| Hyperprotein | 4 | 25 |
| * Mean and standard deviation ** The count is greater than 15, since one patient had a hypocaloric and hyperprotein diet | ||
After the intervention, the results obtained were: for body weight, 84.3 ± 17.6 vs. 76.8 ± 15.9; for BMI, 30.4 ± 5.14 vs. 27.7 ± 4.8; the evaluation of the other parameters is presented in Table 2.
Table 2. The mean and standard deviation of the anthropometric parameters and blood pressure are shown before and after the intervention.
| Before | After | P value | |
|---|---|---|---|
| Weight | 84.3 ± 17.6 | 76.8 ± 15.9 | < 0.001 |
| BMI | 30.4 ± 5.14 | 27.7 ± 4.8 | < 0.001 |
| Abdominal circumference | 99.8 ± 10.6 | 92.1 ± 8.6 | < 0.001 |
| Waist-hip ratio | 0.9 ± 0.05 | 0.8 ± 0.05 | < 0.001 |
| Systolic blood pressure | 149.3 ± 18.2 | 128.0 ± 13.7 | < 0.001 |
| Diastolic blood pressure | 83.6± 7.1 | 74.0 ± 6.3 | < 0.001 |
The results for lipid profile are shown in Table 3; as well as the results of the cardiovascular risk obtained according to the Framingham table and the risk indices for coronary heart disease.
Table 3. Before and after parameters of lipid profile, cardiovascular risk and risk indices for coronary heart disease.
| Before | After | P value | |
|---|---|---|---|
| HDL cholesterol | 43.7 ± 10.6 | 52.1 ± 11.2 | < 0.001 |
| LDL cholesterol | 153.2 ± 43.8 | 113.7 ± 33.9 | < 0.001 |
| Total cholesterol | 240.0 ± 42.8 | 166.1 ± 35.0 | < 0.001 |
| According to Framingham*** | 12.0% ± 0.094 | 4% ± 0.03 | < 0.001 |
| IREC * for combined sexes | |||
| High | 10 (66.7%) | 0 (0%) | 0.007 |
| Under | 5 (33.3%) | 15 (100%) | |
| IREC ** for combined sexes | |||
| High | 9 (60%) | 0 (0%) | 0.012 |
| Under | 6 (40%) | 15 (100%) |
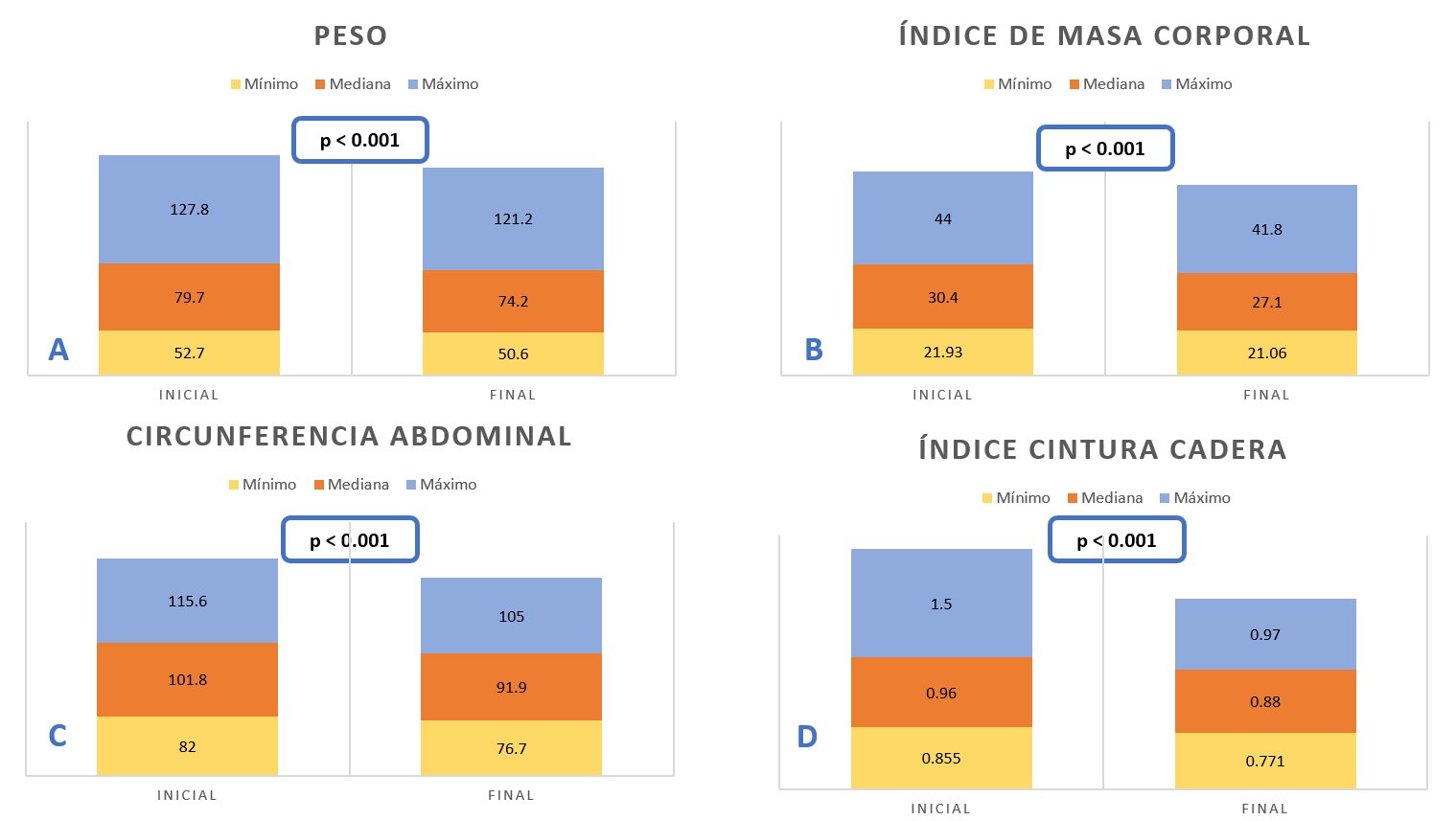
A. Weight before and after the intervention.
B. body mass index before and after the intervention.
C. Abdominal circumference before the intervention and after the intervention.
D. Waist-to-hip ratio before the intervention and after the intervention.
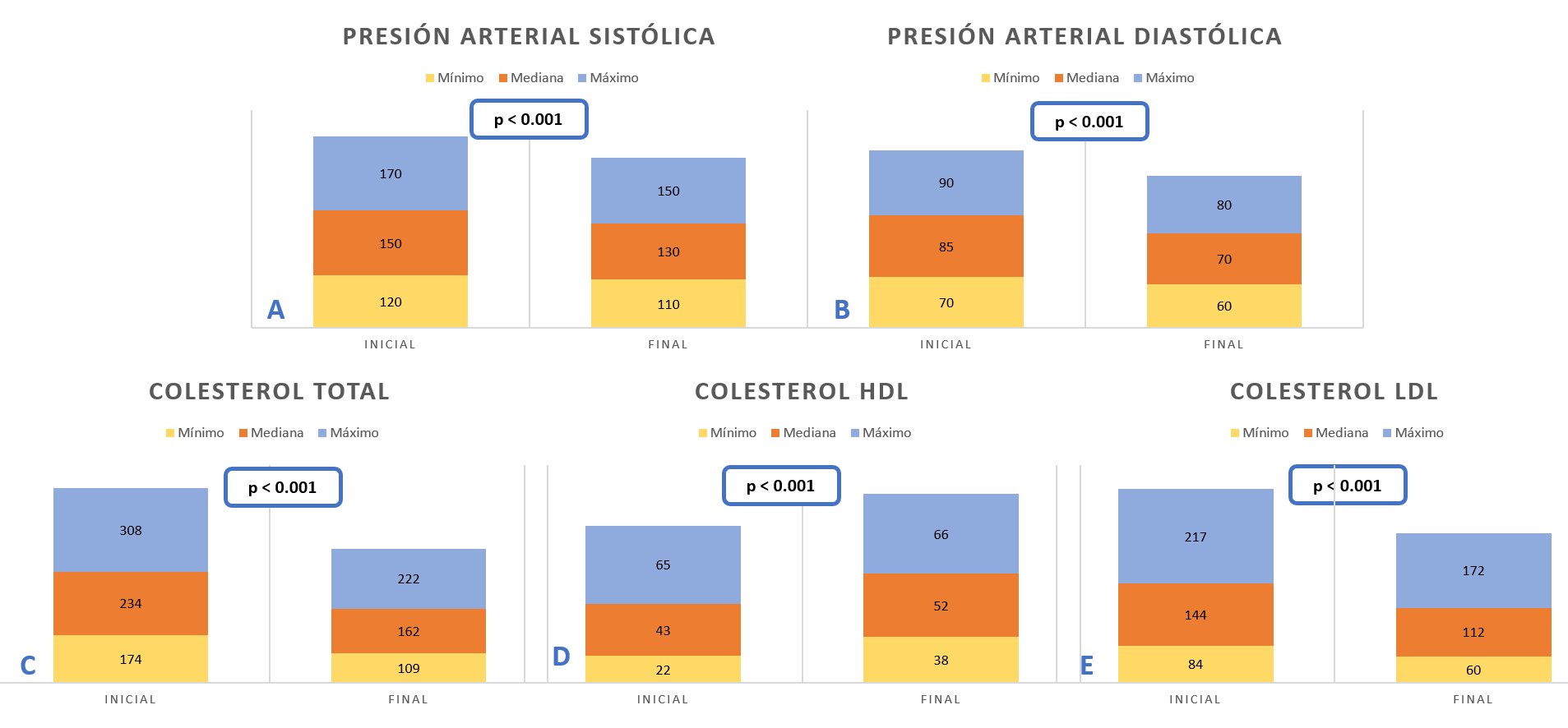
A. Systolic blood pressure before the intervention and after the intervention.
B. Diastolic blood pressure before the intervention and after the intervention.
C. Total cholesterol before the intervention and after the intervention.
D. HDL cholesterol before the intervention and after the intervention.
E. LDL cholesterol before the intervention and after the intervention.
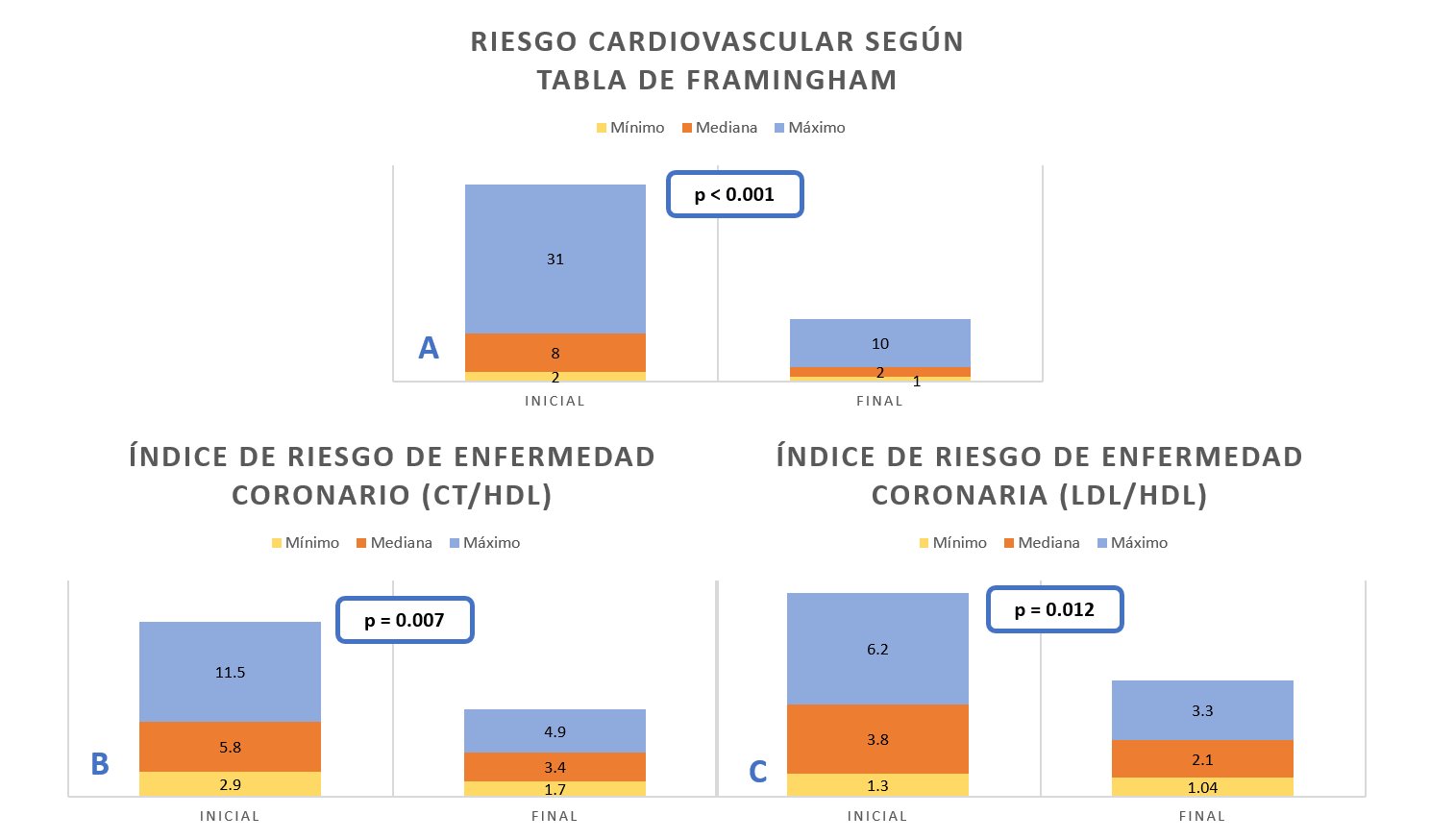
A. Cardiovascular risk according to Framingham before the intervention and after the intervention.
B. I.R.E.C * (Total cholesterol / HDL index) before the intervention and after the intervention.
C. I.R.E.C ** (LDL / HDL Index) before the intervention and after the intervention.
DISCUSSION
The presentation of these series of clinical cases indicated that the 16/8 intermittent fasting scheme
has an impact on the factors evaluated such as weight, BMI, CHF, abdominal circumference, T-c, HDL-c,
LDL-c, R.C. and I.R.E.C. in a variable way in each of the participants, the latter is related to the
type of diet carried out. It is very important to highlight that, although in all reported cases a
reduction in cardiac risk has been seen, in the case of one of the participants this decrease is much
more noticeable (31% vs. 10%), this is probably due to the marked reduction in both your systolic and
diastolic blood pressure; as well as, the decrease in total cholesterol.
Regarding the I.R.E.C., in most of the participants a reduction of the indices was found for
both c-T / c-HDL; as well as for LDL-C / HDL-C; Likewise, authors such as Camelo et al.(7), Peterson.(8), Malinowski et al.(9) Haiyan(10), demonstrated through their studies
the reduction of the values within the lipid profile. The latter is also a risk factor for contracting
cardiovascular disease. Therefore, the application of some intermittent fasting scheme would help to
reduce the values within said profile; and, consequently, the reduction of the risk of some
cardiovascular event.
In relation to body weight and BMI, the fifteen participants presented a reduction in these
values, the most striking case being in one of them (92 Kg vs 78.9 Kg.) And (30.04 Kg / m2 vs 25.75 Kg /
m2), which In addition to the 16/8 intermittent fasting scheme, he consumed a hypocaloric and
hyperprotein diet.
When conducting an exhaustive review, it was found that authors such as Rosa Fernandez et
al.(11), Harris et al.(12), Johnstone.(13), Tinsley and La Bounty.(14), Antoni et
al.(15), among others, demonstrate in their studies the impact from
intermittent fasting versus the fight against overweight and obesity; which today have become a
worldwide evil, being one of the main causes of contracting cardiovascular disease. His studies showed
that intermittent fasting is a good method to reduce the weight of the individual; However, it must
consider the effort that this practice entails; since it has been shown that during the first weeks the
adaptation process will be complicated and is the main cause of abandonment of this approach to
lifestyle.
Regarding the evaluation of CHF and the measurement of the abdominal circumference, all the
participants showed reduction; However, the reduction in CHF was much more marked in one of them (1.5
vs. 0.97) and that of abdominal circumference, in another (115.6 vs. 97.8); the latter consumed a
hypocaloric diet. This reduction could in turn be related to the decrease in coronary risk. Authors such
as Mukai et al.(16), Ahmet et al.(17), Ramasamy et
al.(18) highlighted the benefits obtained in their studies on the heart.
During the evaluation of systolic and diastolic blood pressure, a reduction was observed in most
of the participants, which, at the time of their evaluation, could be classified as arterial
hypertension; or maintenance of blood pressures when the participant was in the normal range. In two of
the participants, a significant reduction in SBP was observed (150 mmHg vs. 110 mmHg) (170 mmHg vs. 130
mmHg), respectively. Tinsley and Horne.(19), Mattson et al.(20) evidenced the impact on blood pressure, demonstrating its reduction
during their study.
When assessing the lipid profile, in the fifteen participants it was possible to see a reduction
on the c-T values. Regarding LDL-C, 14 of the participants showed a reduction in values. Authors such as
Meng et al(10) point out that intermittent fasting is effective for
controlling the lipid profile; however, he emphasizes that in relation to HDL it does not show a
significant effect, but suggests that a further study be carried out.
Some aspects that require special attention of this approach within lifestyle medicine could be
the difficulties and peculiarities of its application; that is to say, its application may not be
adjusted to the reality of all patients; therefore, there must be very clear selection criteria for
patients who are candidates for this approach; for example, those who suffer from severe hypertension,
kidney disease, high LDL levels, high uric acid levels, and type 1 diabetes mellitus may have
contraindications; which does not occur in individuals with type 2 diabetes mellitus. (21)
It is important to emphasize, then, that the benefits of intermittent fasting on the
cardiovascular system are varied and with its application many of the patients who are within the risk
group, with the exception of those previously mentioned, would find a possibility of improvement in his
life style.
The main limitations were the difficulty in data collection and mobilization to obtain them,
because during the time interval taken to carry out the study, it combined with the world situation due
to COVID-19. Furthermore, the adjustment for type of diet is not being considered and there is no group
for comparison.
CONCLUSION
Although the application of intermittent fasting as a contingency plan against cardiovascular diseases requires many more studies. It is concluded that the intermittent fasting scheme showed a significant reduction in anthropometric measurements, lipid profile and blood pressure, and cardiovascular risk. Additionally, an increase in HDL-cholesterol was observed in the sample studied.
Acknowledgments: to Dr. Jhony De la Cruz, director of the Research Institute in
Biomedical Sciences FAMURP, Professor of the Doctorate in Oncology and Research, University of
Palermo, Italy, President Latin American Lifestyle Medicine Association, for the facilities to
carry out this research of the cases and clinical contributions.
Authorship contributions: JAQ has participated in the contribution and data collection.
Funding sources: Self-financed.
Conflicts of Interest: The authors declare that they have no conflicts of interest in the publication of this article.
Received: November 1, 2021
Approved: December 15, 2021
Correspondence: J. Javier Wong – Gonzales
Address: Jr. Manco II Con Calle Padre Urraca N° 120 – San Miguel – Lima, Perú
Telephone number: (+51) 959859575
E-mail: jwongautor@gmail.com
REFERENCES
